You’ve heard this before:
“If kids just ate better and moved more, we wouldn’t have a childhood obesity problem.”
You’ve probably also heard:
“Let’s wait and see—maybe they’ll grow out of it or grow into it.”
But here’s the truth: obesity is a chronic, complex, and progressive disease—and until now, Canada’s national guideline for pediatric obesity hadn’t been updated since 2006. This has made it difficult for healthcare professionals to respond with the same care, urgency, and evidence-based support we bring to other chronic conditions.
That changes today.
Introducing a new guideline, and a new conversation
Managing obesity in children: a clinical practice guideline is the first update in over 20 years, and was published today in the Canadian Medical Association Journal. It’s not just a list of recommendations—it’s a call to do better.
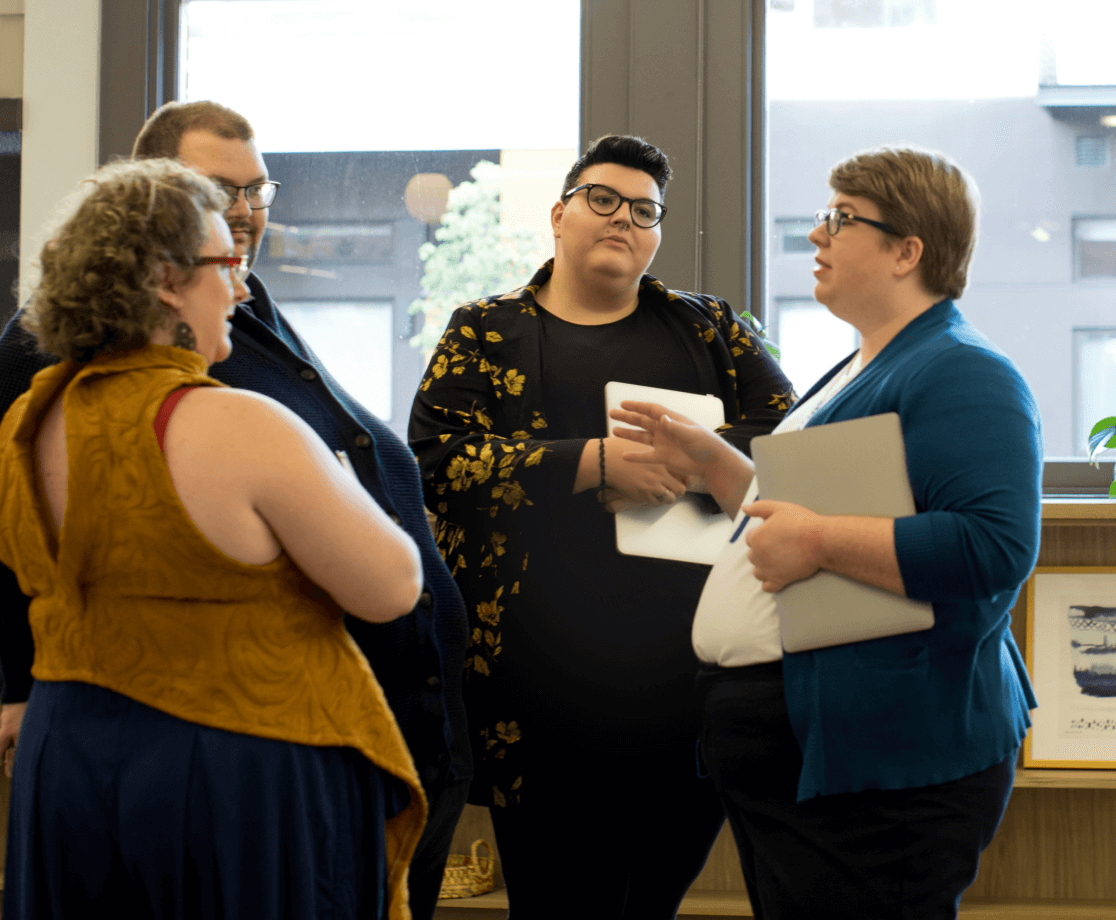
Developed over four years—with input from youth, caregivers, and more than 50 clinicians and researchers—the guideline gives healthcare professionals an evidence-informed foundation to support children and adolescents living with obesity.
Here’s what sets it apart:
- It shifts the goalposts: The focus isn’t on weight loss. It’s on improving health, emotional well-being, and day-to-day quality of life.
- It respects children and families as decision-makers: Shared decision-making isn’t a bonus. It’s the standard.
- It confronts weight stigma: Because the harm caused by bias, especially in clinical settings, is real, and it starts young.
- It recognizes that no two patients are alike: Treatment plans (behavioural, psychological, pharmacotherapy, and surgical) must be tailored to individual needs.
Why this matters now
Childhood obesity often continues into adulthood and raises the risk of more than 200 downstream health conditions. But the impact goes beyond physical health.
Many children living with obesity today also face significant mental health challenges like anxiety and depression—and too often, they experience bullying and hurtful social interactions. Even more critically in healthcare settings, stigma and bias can get in the way of the respectful, empathetic, and evidence-based care every child deserves.
Waiting doesn’t help. Blame doesn’t heal. And shame doesn’t motivate lasting change.
While this guideline focuses on children, we can’t ignore what happens when obesity goes untreated into adulthood. The cost of inaction on treating obesity in Canada is already staggering—economically, socially, and personally.
In Canada, untreated obesity in adults is projected to cost our healthcare system over $120 billion between 2023 and 2075. That figure doesn’t even account for the human cost: reduced quality of life and the deepening impact of stigma over time.
It underscores what this new pediatric guideline is all about: acting earlier, with compassion and evidence, to change the trajectory—for individuals and for our system.
See more about the cost of inaction →
Better care for kids starts with better tools for professionals
This new guideline is about putting tools into the hands of those who need them most: the professionals who support families, the teams designing care pathways, the people who know change is possible when we start by listening.
Read more about the Canadian Pediatric Obesity Clinical Practice Guideline →