6 Years ago today was a bit of a milestone for me. I was out of bed with a bag packed at 5 AM, waiting nervously for my dad to pick me up and drive me to the hospital for my bariatric surgery. I was sick, really sick. My obesity was sucking the life out of me and I was at a point where I was worried I wouldn’t be around for my kids (4 and 2 at the time). To my academic brain, the decision to have bariatric surgery was a simple one. Looking at the evidence, the procedure is the gold standard in obesity management. It is the most effective treatment with the greatest long term outcomes and my best chance to be the dad I wanted to be. To the rest of my brain, it was the most difficult decision I have ever made. It is the most invasive and life-altering of the treatments available. Like any surgery, bariatric surgery is not without risk, while it is relatively safe, as someone going through the procedure there is always a little bit of worry. I was both excited about the hope I had for the future while also petrified that I might be making a mistake.
Fast forward 6 years and I would tell you it was one of the best things I have done for my health and I have no regrets aside from letting my disease progress so far in the first place without seeking help. I am happier, healthier, more productive, more energetic, funnier, smarter and stronger because I decided to treat my disease. Most importantly, I am alive, which 6 years ago I questioned if I would be.
One of my favorite measuring sticks is my kids. After all, the parent I wanted to be, and the way they remembered me was the driving motivation for me doing this. Pre-op Ian was a silly daddy who loved his kids but was often too tired or sore to be the fun active dad I should have been. Pre-op Ian wasn’t overly happy with himself and was often distracted meaning I couldn’t give my kids the attention they deserved, was sometimes grumpy and just not the role model I wanted to present to them. Now 6 year post-op Ian is still a silly daddy who loves his kids, I however have the energy to be sillier. I can be that active dad I wanted to be. I have learned to love myself more and am much happier for it (I will say, this is not because of the weight loss, more so the journey and what I have learned along the way). I am still distracted sometimes, but not because of my health, more for the normal work/life stresses we all face.
I went from having a hard time finding the drive to take my kids to their extracurricular activities like sports, to now being a coach. Last year I was the head coach for my son’s hockey team and baseball team and I also helped out as an assistant for my daughter’s hockey and baseball team. Last season between both kids, I was on the ice making memories 4 days a week! This is my measuring stick of how successful my obesity treatment has been and it has nothing to do with the scale.
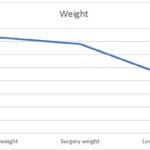
You will not often find me discussing my weight. I am very deliberate in my effort to not add to the toxic weight loss scale obsession, and for good reason, weight is not a valid or reliable measure of health or success in obesity management. So, I will break some of my personal rules for the sake of demonstration here. This graph shows you my post-bariatric 6 year weight loss:
Now, with our traditional thinking, this looks impressive. 6 years out I have lost 130 lbs. WOW! Right?
Nope, not so fast, this chart doesn’t tell you any of the story, it doesn’t tell you how my health has improved. It doesn’t tell you about how hard it has been, it doesn’t tell you about how working on one problem triggered others that needed attention, it doesn’t tell you about my regain and subsequent additional obesity treatments and it certainly does not tell you about my growth and all I have gained over this time.
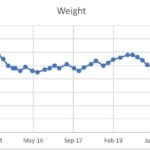
Here is a slightly more detailed chart:
As you can see, it is not a straight line, lots of ups and downs and fluctuations.
After my surgery a few things happened. I lost an insane amount of weight that I could have only dreamt of previously. It took a while to adjust but overall, I felt great and had good energy levels. My hypertension got to the point where I did not need medication anymore. I no longer needed my C-PAP for my sleep apnea, blood work all looked great. A booming success! My body also adapted to this massive weight loss, and in attempt to survive, made some changes I couldn’t see but I could feel. Around 2.5 years post op, the resistance began. Up until that time, surgery was a miracle, I was never hungry and I never really had to think about food. But as part of the natural physiological response to weight loss, I gradually lost that superpower. My food brain gradually crept back in, consuming my thoughts and driving cravings, hunger cues and never really feeling full. However, this time it was so much worse than it was before surgery. Food became the only thing I could focus on. From the moment I woke up to the moment I went to sleep food was in my thoughts. What could I eat, where was I getting it, what could I eat without others noticing, if I go shopping what can I pick up on the way, what could I snack on the way home, with the ingredients in my house what could I put together. It was obsessive, it was distracting and it was all consuming. I had no brain power left after fighting these thoughts and cravings all day. As you can see in the chart above, my regain shows the effect of that.
I was desperate not to go back to being sick the way I was pre-op, and I had to remind myself that surgery is but one tool in the toolbox and certainly not a cure. I threw myself into learning more and working towards better management of my disease. I returned to my surgical team and talked to my dietitian and nurse. I got a referral to the psychiatrist and started seeing a counselor, I read books on food and the brain, addiction, mental health and personal well-being.
I was sure that the mental health side of this was a missing piece that I was not managing well. Being able to talk about these issues opened me up to reflection and a much better understanding of my disease. Perhaps the most important take away was my appreciation for the value of self-love and the need for self-care that is decoupled from the scale. Slowing down, enjoying a bit more, reflecting more, saying no. These all helped me immensely. I also discovered that I had undiagnosed ADHD symptoms and anxiety and continue to work on that.
I got a referral to an obesity doctor outside of my bariatric program (and I fully acknowledge my privilege living where I do and having access to such people, knowing many do not). With this doctor I learned a great deal about the brain and it’s involvement in obesity and specifically in regain. This helped to explain why my brain was consumed with food an uncontrollable food drive and why I was having such a hard time with it. The study of food addiction really helped me with this and what rounded out my obesity management was the use of medication. This combination of medicine, working on my mental health, developing strategies through cognitive behavioral therapy and learning about addiction has now made my toolbox a well-rounded one that has me better prepared for the work ahead.
So from a 6 year bariatric surgical post-op, here are a few of my top reflections from my experience:
- I have been asked if I feel like I cheated or took an easy way out by having surgery. To that I say no because this was not easy at all, but for the sake of argument and to push back on that common narrative surrounding obesity treatments, I would say even if it was cheating, if it came to your health and wellbeing, wouldn’t you cheat? I would, every single day and twice on Sunday.
- The change in my body highlighted issues in my head that needed to be addressed and these were things that were not as obvious pre-op. I don’t want to say the surgery caused these issues but it helped to reveal another layer of my health that needed some attention, I am grateful for that challenge and awareness. Never discredit the need to work on your head alongside your physical health.
- I still see the old me. My body has changed and I look different but some days I struggle with still seeing the bloated, sick version of myself in the mirror. I am still uncomfortable in my skin and not always happy with myself. I have a fierce battle with imposter syndrome that I wage in regularly, but I am more aware of it now, I can acknowledge it and not let it impact me the way it did.
- My health and wellbeing needs to be a priority for me to be the person I want to be. If I want to be a good husband and father, I need to make sure I take care of me. By investing in my self-care, I have more to give to those I love.
- Honesty is key. The more honest I was with myself and others about my health and issues, the better my care was. I was better prepared to ask questions of health professionals, I was better prepared to receive advice. I also found talking about it openly helped me understand that I am not as unique as I once thought. There are many others who understand and share similar experiences. Finding my people and being open has been the single most important component of my obesity management.
Six years ago today I was scared out of my mind in a hospital, today I am writing this post healthier and happier than I remember being as an adult. While the hope for the future was made possible by the surgery, I now recognize how small of a part that surgery played in the grand scheme of my health when you consider the rest of the journey that has taken place since then.