Today’s blog post has been written by Jennifer Brown, MSc., RD, CBE
A proof-of-concept project that implements the Canadian Adult Obesity CPGs into practice.
“Individuals living with obesity are subjected to weight bias, stigma and discrimination, particularly evident from the healthcare system, including healthcare providers, the physical environment including equipment or safety, and access to treatments and/or services within the healthcare system.”
According to the Canadian Adult Obesity Clinical Practice Guidelines (CPGs), healthcare providers and healthcare systems should recognize obesity as a chronic disease, defined by excess or abnormal body fat (adipose tissue) that impairs health. Healthcare providers (HCPs) should be aware of their own attitudes and behaviours towards individuals living with obesity and those with higher body weights or larger bodies. And, HCPs should not assume that all individuals with larger bodies or higher body weights, have the disease of obesity.
Furthermore, assessment of obesity should be comprehensive, individualized and address root causes and systemic barriers. Body mass index (BMI) is not recommended as a diagnostic tool at the individual level and HCPs should receive updated training on the complex interplay between genetic, biological, psycho-social, and environmental factors. Treatment exists for adults diagnosed with obesity which should include individualized medical nutrition therapy and physical activity as adjunctive therapies to interventions that target biological and environmental factors affecting obesity, including psychological, pharmacological and surgical interventions. Goals of treatment should be person-centred, value-based and focused on improving health and quality of life, not weight loss alone.
Lastly, HCPs and healthcare systems should ensure physical environments, equipment, assessment methods and access to treatments are universal across all sectors in Canada, whereby people are treated with the same dignity, respect and care that anyone would expect, regardless of body weight, size or health condition.
What’s the problem?
Clinical Practice Guidelines are often developed to improve quality of care, support clinical practice, improve patient outcomes and influence health system outcomes. Many Clinical Practice Guidelines can be transferable across multiple chronic diseases but yet, oftentimes, they are not integrated by clinicians, organizations or agencies, leading to inconsistent care, risk of harm and increased cost to healthcare systems.
When the Canadian Adult Obesity Clinical Practice Guidelines (CPGs) were published in 2020, they were the first patient-centered guidelines to address weight bias/stigma for adults living with obesity and a pioneer in shifting the narrative of obesity to focus on health-based outcomes instead of weight or BMI (read here and here for more highlights of the CPGs). For years, people living with obesity and those with larger bodies or higher body weights have been shamed, blamed and discriminated against because of their weight, often resulting in health inequalities and less access to services or healthcare. The CPGs were paramount in providing recommendations to patients, healthcare providers and policy makers to acknowledge and mitigate weight bias, stigma and discrimination within the healthcare system and clinical practice.
What’s the uptake?
The CPGs have been endorsed and recognized, nationally and internationally. They were the most read article from the Canadian Medical Association Journal in 2020-2021, at a time when COVID-19 was the number one global concern. The CPGs have made over 85 million media impressions from over 300 unique reports and have reached over 120,000 health professionals through CPG webinars, presentations and/or conference meetings. Countries all over the world have praised the Canadian CPGs and a recent pilot project found that it is possible to adapt the Canadian Adult Obesity Clinical Practice Guidelines for different health systems and populations, while reducing time, costs and maintaining the scientific validity of the guidelines. This uptake of the CPGs has been done internationally, within Ireland and Chile, with more countries following suit, however, little is known or documented on the uptake of the CPGs in Canada.
Proof-of-Concept in Canada
In 2021, the University of Ottawa Heart Institute (UOHI) collaborated with Obesity Canada (OC) to conduct a proof-of-concept project by implementing the Canadian Adult Obesity Clinical Practice Guidelines (CPGs) across their organization.
The objective of this project was two-fold; (1) to update resources, practices and the clinical environment to be consistent with the key messages and evidence-based recommendations from the Canadian Adult Obesity Clinical Practice Guidelines (CPGs); and (2) to produce an implementation tool kit that stakeholders could implement across federal, provincial and territorial jurisdictions. Furthermore, the collaboration and novel approaches used in the project would serve as a proof-of-concept in the development of a National Obesity Care Framework.
How we did it
The UOHI collaborated with OC by contracting an expert representative to facilitate various quality improvement (QI) projects identified by an interdisciplinary committee (including patient advocates, clinicians, students, management and external experts) to ensure messages and content was aligned with the CPGs. The process was documented to serve as a proof-of-concept for the National Obesity Care Framework and an implementation toolkit is in development to support stakeholders across Canada replicate the process. The UOHI also joined the Canadian Obesity Advocacy Network (COAN), a diverse group of over 20 organizations that are united with the purpose of changing the narrative of obesity in Canada.
The QI projects incorporated 17 evidence-based recommendations and various key messages from 8 chapters of the CPGs for both patient and healthcare providers, emphasizing the following three themes:
- Increase knowledge and education for patients and healthcare providers about obesity and weight bias/stigma
- Change attitudes, beliefs and practices of healthcare providers working with individuals living with obesity and/or individuals with larger bodies.
- Provide a safe and accessible environment for patients to discuss obesity across the care continuum
Best-practice frameworks guided the development and implementation of the overall project and results of various QI projects have been or are in the process of being published. Examples of QI projects include:
- Bariatric accessibility and equipment – created an inventory of existing and required equipment for patients and family members with bariatric needs using Obesity Canada’s Bariatric Friendly Health Care resources, Alberta Health Services Bariatric Friendly Hospital resources and evidence from the CPGs chapter on Activities of Daily Living. Provided weight bias and safety equipment training for staff to identify individuals with bariatric needs.
- Professional development and training – provided education and training opportunities for healthcare professionals and staff within the UOHI.
- Patient and healthcare provider resources – created videos and pamphlets on obesity and weight stigma, changing the narrative of obesity as a chronic disease and not a lifestyle choice.
- Website communication – identified, removed and/or revised content to be consistent with the CPGs.
- 5A’s pilot project – updated health assessment forms within an outpatient cardiac rehabilitation setting to be aligned with assessment recommendations and the 5A’s to obesity management (ask, advise, assess, agree and assist) of the CPGs.
What will this mean?
Obesity is still not well understood. It is still viewed by some as a lifestyle choice, an individual’s responsibility, and is often seen as a simple solution of just ‘eating less and moving more’ or choosing healthier foods and not being lazy. These assumptions are unequivocally incorrect and have perpetuated years of harmful health behaviour practices, self-blame and inequitable access to tests, procedures and/or treatments for health conditions associated with weight or body size.
The UOHI/OC proof-of-concept project changes these assumptions by acknowledging existing biases, recognizing gaps in HCP knowledge and training, identifying inconsistent language or messaging about obesity and associates the gaps in physical, clinical and policies to inadequate healthcare delivery. They have used an interdisciplinary and multi-sectoral approach that brings together individuals with lived experiences, clinicians, researchers, managers, decision makers, experts and community members to support the changing narrative of obesity.
Creating an implementation toolkit that other stakeholders across Canada can utilize has the potential to address the inequities previously mentioned. It may also prove to be cost effective by standardizing messaging, education, healthcare practices, treatments, and most importantly, ensure the respect and dignity of individuals living with obesity.
What you can do
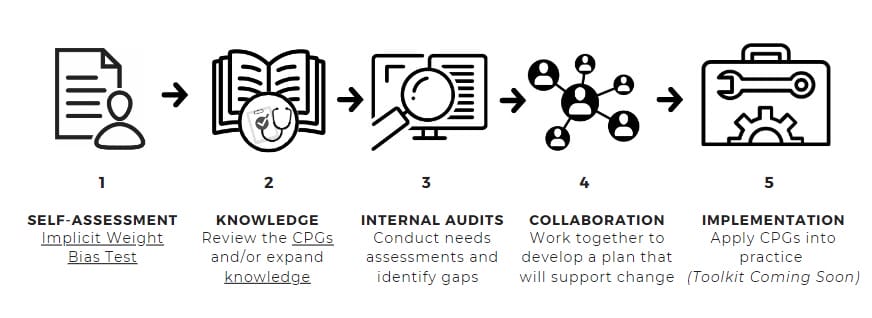
We can all start by acknowledging our own biases, oftentimes, biases we don’t even realize we have. There are self-assessment tests like the Implicit Association Test for Weight Bias that we can all take. From there, we can be open to challenging our beliefs, our practices and/or our knowledge about obesity. We can look at our resources, communication tools and/or messages within our practice or organizations to assess whether the information is updated to reflect the evidence and key messages from the CPGs. We can collaborate with multiple groups, people with lived experiences, interdisciplinary members that have various interests in obesity and weight stigma (contact Obesity Canada for patient and/or expert support). And, lastly, once available, we can use the UOHI/OC Implementation Toolkit as a guide to implement assessments, processes, resources and examples of implementation strategies.
Change takes time and requires a collaborative, multi-stakeholder approach, which is why this pilot project between the UOHI and OC can serve as a beacon of progress that organizations, agencies, and governments can implement. For more information or if your organization would like to follow the example of the UOHI, please contact us.






