EDMONTON, August 4, 2020 – Canadians living with obesity and the healthcare professionals who support them have a new roadmap for quality collaborative care.
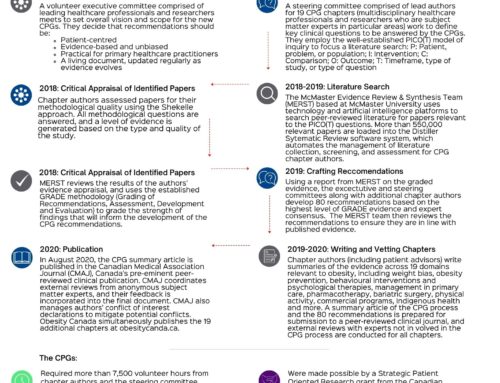
More than two years in the making, the Canadian Adult Obesity Clinical Practice Guidelines (CPGs) provide a much-needed evidence- and experience-based, patient-centred framework for healthcare professionals, patients and policy makers. They represent the first comprehensive update in Canadian obesity guidelines since 2007, and perhaps the most extensive review of published evidence yet conducted in obesity worldwide.
Developed by Obesity Canada and the Canadian Association of Bariatric Physicians and Surgeons, the new CPGs were authored by more than 60 Canadian health professionals, researchers and individuals living with obesity. Together, they assessed well over 500,000 published peer-reviewed articles and built consensus on a wide range of clinical and scientific issues to identify 80 key recommendations.
“Science tells us the drivers of weight gain are complicated and unique to the individual, and also that the human body is hard-wired against weight loss. Historically, we have told people whose weight affects their health merely to eat less and move more, which on its own is ineffective and even dangerously simplistic advice,” says Dr. Arya M. Sharma, scientific director of Obesity Canada. “The CPGs represent a turning point in the way Canada needs to approach the treatment of obesity, and that is to acknowledge obesity as a complex chronic disease requiring lifelong support, as we do for diabetes, heart disease and others – this is the best evidence to date on how to do that.”
The CPGs are rooted in patient-centred care, with patients and providers working together to identify personal drivers of obesity, set realistic goals and maintain healthy behaviours over the long term. In addition to medical nutrition and physical activity, psychological interventions, medications, and surgery can be used to support patients as needed. The CPGs also discuss key issues such as weight bias, implications for Indigenous communities and more.
“People who live with obesity have been shut out of receiving quality healthcare because of the biased, deeply flawed misconceptions about what drives obesity and how we can improve health,” explains Lisa Schaffer, Chair of Obesity Canada’s Public Engagement Committee. “Obesity is widely seen as the result of poor personal decisions, but research tells us it is far more complicated than that. Our hope with the CPGs is that more healthcare professionals, health policy makers, benefits providers and people living with obesity will have a better understanding of it, so we can help more of those who need it.”
A summary of the recommendations was published today in the Canadian Medical Association Journal online at https://www.cmaj.ca/lookup/doi/10.1503/cmaj.191707, and 19 in-depth chapters are available online on the Obesity Canada website at www.obesitycanada.ca/guidelines. The 19 CPG chapters will be an open-source, living document that will be updated as new evidence emerges. The CPGs were supported through a Canadian Institutes of Health Research Strategy for Patient-Oriented Research grant.
For more information or to arrange interviews with CPG authors, contact Brad Hussey, Communications Director, Obesity Canada via hussey@obesitynetwork.ca / 905-628-7778 (ET).
About Obesity Canada
Obesity Canada-Obésité Canada is Canada’s authoritative voice on evidence-based approaches for obesity prevention, treatment, and policy. Our mission is to improve the lives of Canadians affected by obesity through the advancement of anti-discrimination, prevention, and treatment efforts. www.obesitycanada.ca
About CABPS
The Canadian Association of Bariatric Physicians and Surgeons (CABPS) represents Canadian specialists interested in the treatment of obesity and severe obesity for the purposes of professional development and coordination and promotion of common goals. https://cabps.ca/