Individuals living with obesity or individuals living in large bodies report challenges accessing health care services in institutional and community settings that meet their needs. Key issues identified include access to equipment and furniture that will support their body weight and/or body size; limited knowledge about bariatric care needs and; weight bias and stigma from health care practitioners.
Patients with obesity are at higher risk in hospital settings for injury, complications and longer in-hospital stays due to inadequate facility design, equipment, or staff competencies in their care. Healthcare providers are also at risk for injury if there is inadequate equipment, as well as the knowledge to use the equipment.
These resources have been curated by Obesity Canada and developed in collaboration with members of the OC community, organizations and health authorities. The following is a high level summary of tips, strategies and resources. Links to full reports, guides and tools are included throughout this page. The resources and recommendation on this site are intended to promote quality care for patients who have bariatric care needs.
Creating Hospital and Long-term Care Settings that Meet Bariatric Care Needs
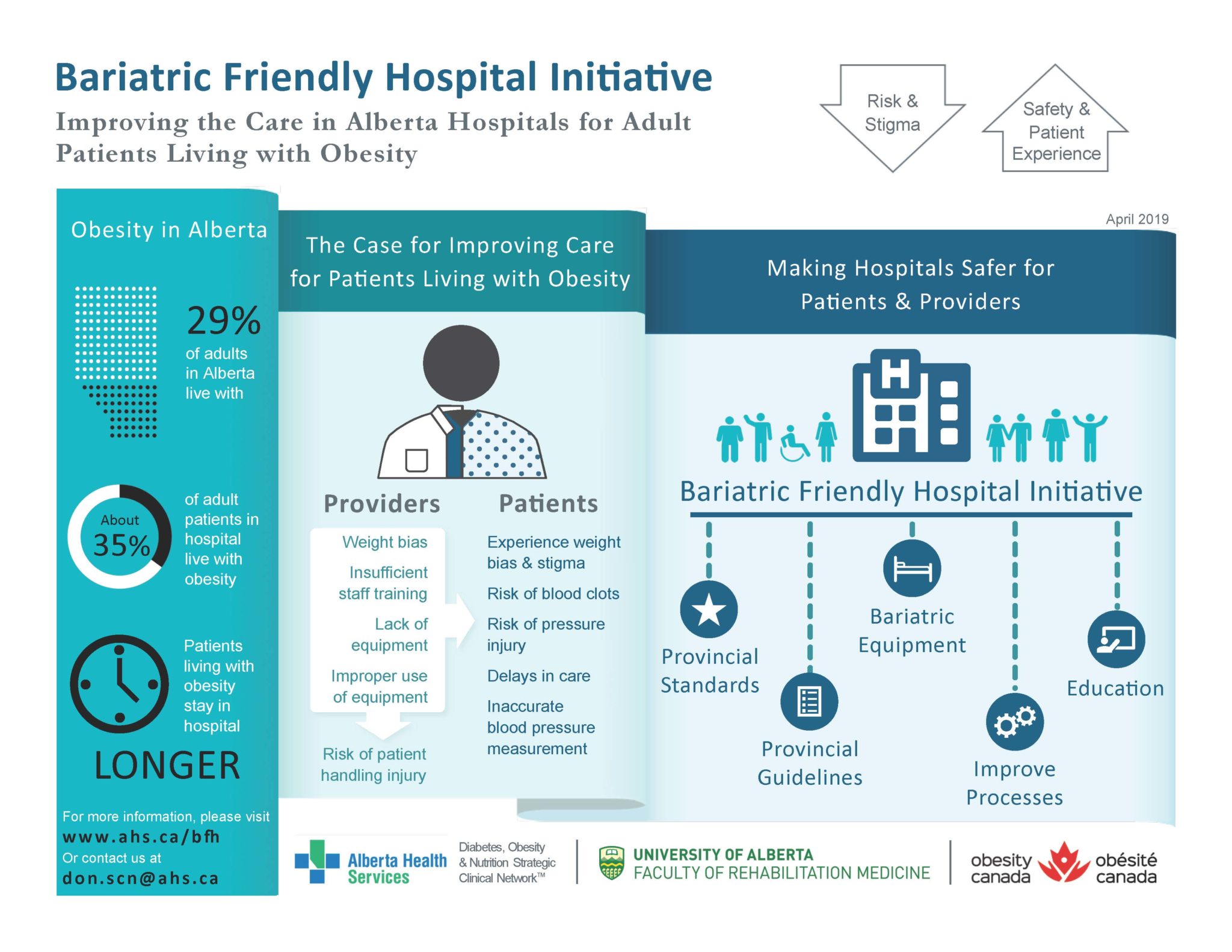
Over the past decade, progress has been made by several groups of healthcare professionals and designers to create rooms in hospitals that are safe and accessible for patients with bariatric care needs and the staff that work with patients. The Bariatric Friendly Hospital Initiative, a collaboration with The Faculty of Rehabilitation Medicine at the University of Alberta, Alberta Health Services Diabetes, Obesity and Nutrition Strategic Clinical Network and Obesity Canada, has pulled together a list of resources and recommendations to promote quality care for hospitalized patients with bariatric care needs.
The following are summaries of the content. The full document can be accessed with this link: Bariatric Friendly Hospital Initiative . Health care institutions including hospitals and long-term care centres are encouraged to use this resource and adapt to their local context.
How to identify if a patient has bariatric care needs
The term “bariatric” is typically used when a patient has a body mass index (BMI) of 30 kg/m2 or more. However, the BMI may not be known when decisions about a patients’ care must be made. It is also important to note that BMI does not provide adequate information about a patient to determine their specific care needs. To help identify if a patient has bariatric care needs, it is recommended that the term “bariatric” be used to describe the care needs of a patient who has a body weight of 113kg (250lbs) or higher. The reason for this starting point in body weight is that most equipment/furniture in a hospital, clinic or other type of public space has a weight capacity of 113kg (250lbs). Therefore, patients who have a body weight greater than 113kg (250lbs) may require equipment/furniture that is classified as “bariatric” meaning that it likely has a weight capacity greater than 113kg (250lbs).
Other considerations to determine if a patient may have bariatric care needs is the shape of their body. The location on a patients’ body of accumulations of tissue including adipose and skin will determine the need for equipment/furniture that will accommodate and support the patient to lie down, sit and/or walk.
Bariatric Care Needs Decision Making Algorithm
Together with our collaborators, we have created an algorithm to help health care practitioners identify if a patient has bariatric care needs. It is recommended that this quick and easy to follow process be completed as early as possible in the patients’ admission to the healthcare system.
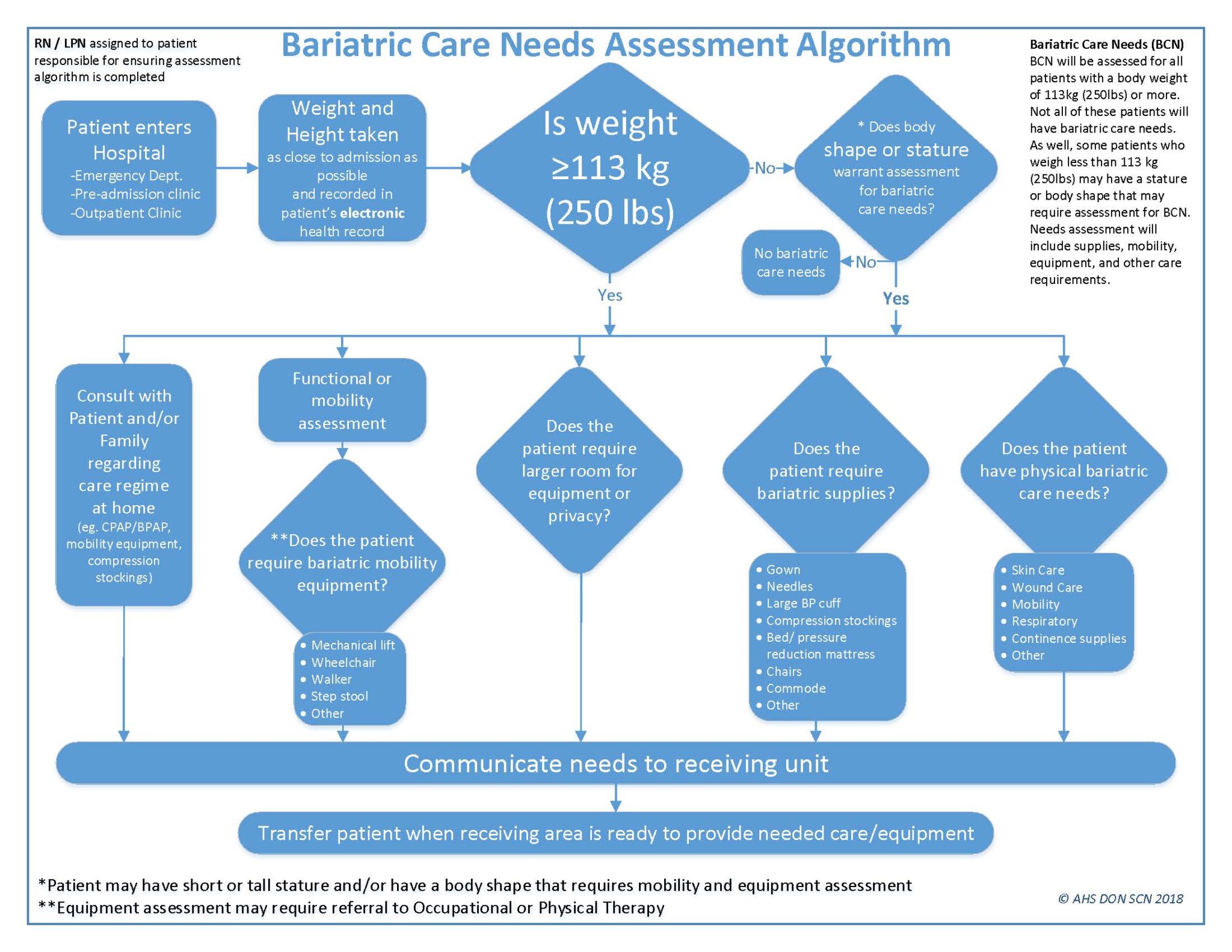
Use the below bariatric care needs assessment algorithm to assist with identifying patients with bariatric care needs.
This comprehensive resource should be used to assist clinicians in providing care for patients living with obesity.
People First Language
Using people first language is now the standard in health care for addressing people respectfully. This means that a person is described as a person first and the name of the chronic condition is used after. In the case of obesity, rather than stating “obese person” or “obese patient”, the statement “person with obesity” or “patient with obesity” is recommended. This small but important change reinforces that obesity is a chronic disease and not a characteristic or adjective. Obesity Canada has a statement about people first language that can be found here https://obesitycanada.ca/resources/people-first-language/ .
Use of Appropriate Images
Images of people with obesity used on-line or in print by members of the media, health care professionals, government, industry, etc. can be a source of stigmatization. Photos often show individuals with obesity as headless (i.e. only from the shoulders down), from unflattering angles (e.g. with only their abdomen or lower body shown), and engaging in stereotypical behaviour (e.g. eating at fast food restaurants or food courts, engaging in sedentary activity). These images degrade and dehumanize individuals with obesity while perpetuating myths and stereotypes.
It is recommended that all on-line and printed material only use images of persons with obesity in ways that are positive and non-stereotypical. Such images are available as a free resource from Obesity Canada via the Image Gallery (www.obesitycanada.ca).
To learn more about the Weight Capacity Labeling system, please email Nicole Pearce.